New Orleans doctor describes success using hyperbaric chambers to treat veterans.
The American Legion’s Post-Traumatic Stress/Traumatic Brain Injury Ad-Hoc Committee was created last October to, according to its mission statement, “investigate the existing science and procedures, as well as alternative methods, for treating TBI and PTS currently being employed by the Department of Defense or Department of Veterans Affairs.”
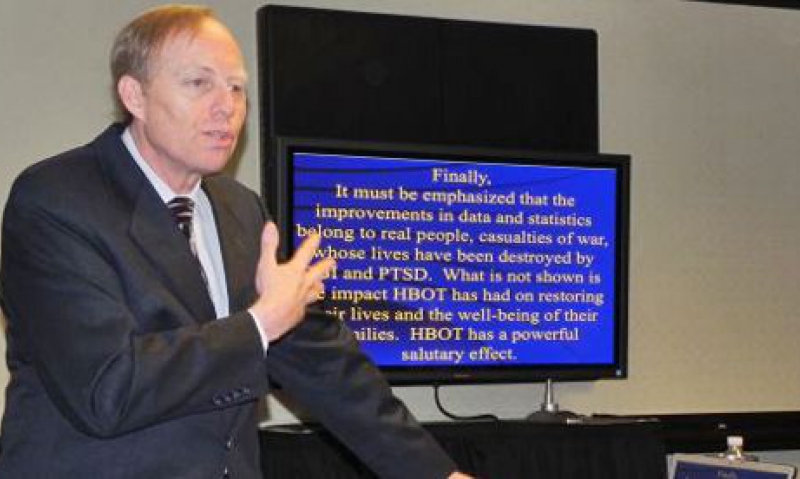
During the Legion’s 51st Annual Washington Conference, members of that committee were given an in-depth presentation on one of those “alternative methods.”
Dr. Paul Harch of New Orleans briefed the committee about his use of hyperbaric oxygen chambers to treat TBI and PTS, commonly regarded as the signature wounds of the war on terrorism.
Harch has used hyperbaric oxygen treatments for dozens of U.S. veterans who suffered injuries resulting in TBI and who have developed PTS. He recently finished up a study on 15 patients who showed improvements in several physical and mental tests after a series of hyperbaric treatments, which involves patients breathing pressurized oxygen inside a sealed chamber.
Patients went through a battery of pre- and post-treatment tests. Test subjects showed an average IQ improvement of nearly 15 points. Thirteen of 15 saw a reduction in headaches, while nine of the 12 who reported sleeping issues cited an improvement. Seven of 11 subjects on prescription medication for their conditions began using that medication less frequently or discontinued use of the medication following the treatment plan.
Harch also used the military’s PTS checklist and scored all of subjects before and after the treatment plan. The subjects showed a 30-percent reduction in how they scored after being treated.
“All of the data and statistics I showed you is necessary,” Harch told the committee. “But these were real people. These were brain-injured men and women whose lives are literally destroyed by these injuries. What is not shown here, and what I can’t quantify, is the impact (hyperbaric oxygen) has had on them and their families.”
Harch cited as an example U.S. Army Reserves Brig. Gen. Patt Maney, who was injured by a roadside bomb in Afghanistan. A judge in Florida, Maney was undergoing cognitive therapy at Walter Reed Army Medical Center that “helped a little bit,” Harch said. But Maney’s condition was still so bad that he was unemployable.
Maney underwent 80 hyperbaric oxygen treatments and is back to the bench in Florida, functioning as a judge once again.
But Maney is just one of several success stories, Harch said. Yet there remains reluctance on the part of DoD and VA to use the procedure for wounded veterans. The primary reason is pretty clear to Harch.
“It’s the price tag,” he said. “I firmly believe that’s No. 1. We charge $200 an hour at our clinic. The Medicare rate is about $275 an hour. This is billed in hospitals at $2,000 an hour. DoD has thrown out a figure that you need $500,000 lifetime to treat a brain-injured veteran for these symptoms and problems. First of all, there’s no evidence for that. Secondly, if you even took the 80-treatment protocol that I developed, that’s $160,000 at the billed hospital rate … The reality is the treatment with drugs and all these other therapies is doubly expensive.”
Harch said the other issue is an out-of-date perception of the procedure.
“What was I taught at (Johns Hopkins University)?” he said. “This is my generation of doctors. We were taught that (hyperbaric oxygen treatment) is a fraud, and the reason is nobody understood how it worked. It got a bad name when it was applied to multiple sclerosis. People stood up and claimed it affected impotence, balding and cancer. There is so much misinformation. In my generation of doctors, we have been led to believe this is a scientifically disproven, fraudulent type of therapy. We’re working against this past body of misperceptions.”
- Washington Conference

